Being a middle school student has its fair share of challenges, even on good days. And for children with Tourette syndrome, these challenges are amplified. Children who experience motor and/or vocal tics struggle with repetitive, involuntary movements and sounds. These can be distracting, uncomfortable, negatively impact self-esteem, and even result in bullying. When tics increasingly interfere with a child’s ability to thrive, comprehensive treatment can help.
What is Tourette Syndrome and What are Tics?
There are two types of tics: motor tics (movements) and vocal tics (sounds). Examples of motor tics include eye blinking, facial grimacing, or leg twitching. Likewise, vocal tics may present as sniffling, grunting, or throat clearing. When a particular tic involves multiple muscle groups, such as extending one’s arm and then making a fist, it is referred to as a complex tic. When an individual has multiple motor and at least one vocal tic, they are diagnosed with Tourette syndrome.
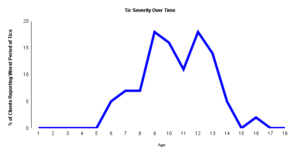
Tics can present differently in each child, but they typically begin as motor tics and a child may later on develop vocal tics. Oftentimes the tics begin in the facial area before moving down to other areas of the body. The severity of tics tend to wax and wane over a period of time and can be impacted by external factors. For example, a child’s tics may be less prominent when they are very focused on an activity. Conversely, they may be exacerbated and become more noticeable in situations of stress, excitement, or fatigue. It is important to note that every child’s tics respond differently to their environment. These tic presentations can vary and may differ from the examples provided here.
CBIT and Treatments for Tourette Syndrome and Tics
While there is no “cure” for tics or Tourette syndrome, there are management strategies. There is extensive research supporting a specialized form of behavior therapy for tics called Comprehensive Behavior Intervention for Tics, abbreviated as CBIT (pronounced as see-bit). CBIT is a first-line intervention for many individuals with Tourette syndrome and tics according to the AACAP, the AAN, and the Tourette Association of America.
Although tics may seem to come out of the blue, a psychologist can help someone learn to detect them before they happen. CBIT is a multi-component behavioral intervention designed to help individuals manage their tics. The core intervention within CBIT to reduce the frequency of tics is called Habit Reversal Training (HRT). The first step in HRT is to teach individuals to become more aware of their tics— specifically, the “warning signs” which immediately precede their occurrence. These warning signs are often referred to as “urges” or physiological sensations that occur just before exhibiting a tic. Next, individuals are taught to engage in a specific behavior which is incompatible with exhibiting the tic. The exact behavior, called a “competing response,” is determined based on the specific tic. The goal of this treatment is to try and teach the brain to resist the urge to tic, even when it thinks that it must act upon it. Over time, the urge to tic may even go away. In addition to HRT, CBIT treatment includes education about tics and their course, strategies to reduce stressful situations which can make tics worse, and occasionally relaxation training.
CBIT can be implemented alone or in conjunction with medication management. For decades, the treatment of choice for tic disorders, including Tourette Syndrome, was medication. While medications can be effective, many parents prefer not to place their children on medications unless necessary, either on principle or due to concerns about adverse side effects. Ultimately the decision to use medication as a treatment approach is a decision that should be made in consultation with the clinical providers involved in your child’s care.
It is important to know that many youth with tics may not be bothered by them. If the tics are not causing any interference at home or at school, the best course of action may be to just wait and
Tourette Syndrome and Co-Occurring Disorders
A significant number of youth with Tourette Syndrome also have co-occurring psychological disorders. The most common ones are attention deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD), followed by other anxiety disorders. It is common for children and adolescents with Tourette syndrome to receive treatment for one or more disorders, even when their tics are manageable or well-controlled with medication or behavior therapy. Oftentimes these co-occurring conditions may be more impairing than the tics themselves. For that reason, many families find it helpful to work with a provider who has expertise in tic disorders as well as the co-occurring conditions.
Supporting Children with Tourette Syndrome
Most importantly, you should never punish a child as a result of their tics. In fact, the stress a child experiences in response to such reprimand will likely make their tics even worse. The best approach for parents and educators who interact with a child dealing with tics is to increase their knowledge about tics and Tourette syndrome. Learning about the course of the disorder, what makes tics worse, and the treatment options available generally helps adults feel much more comfortable around youth with tics. Attending a consultation, workshop, or in-service about tics and related disorders is a great way to do this. A psychologist who specializes in Tourette syndrome and tics can also provide a comprehensive assessment, develop a tailored treatment plan, and offer support for managing co-occurring conditions such as ADHD or OCD. Additionally, they can educate families and school staff about Tourette syndrome, helping to create a more understanding and accommodating environment for the child. These types of interventions often help adults to naturally make meaningful changes to accommodate children with tics and Tourette syndrome.
Living with tics and Tourette syndrome can be challenging, but with understanding, appropriate treatment, and support from family, friends, and educators, children affected by these disorders can thrive. Working with clinical providers well informed on tics and Tourette syndrome can help you increase your awareness and provide a supportive environment for children coping with tic disorders, helping them lead fulfilling lives.